The National Health Insurance Authority (NHIA) has wielded the big stick on 49 Healthcare Facilities (HCFs) and 47 Health Maintenance Organisations (HMOs) for various service failures last year.
It warned that substandard care for enrollees will no longer be tolerated.
This is contained in the Authority’s 2024 Annual Complaints Report, released by the Acting Director, Enforcement, Dr Abdulhamid Habib Abdullahi.
The NHIA, according to the report, investigated a total of 3,507 complaints nationwide last year, resolving 2,929 cases an 84% resolution rate within the standard response window of 10 to 25 days.
It disclosed that common complaints against healthcare facilities included unavailability of medicines, denial of services, out-of-pocket payments for covered treatments, and poor payment narration. HMOs, on their part, faced complaints of delayed or denied referral codes, failure to settle reconciled payments, and poor oversight of service quality.
It also said the enforcement actions saw 84 warnings issued to erring healthcare facilities.
Besides, 54 enrollees received refunds amounting to N4,375,500 from 39 facilities, while four facilities were suspended and six delisted. For HMOs, 35 were issued warning letters and corrective directives while 12 were ordered to refund N748,200 to 15 enrollees.
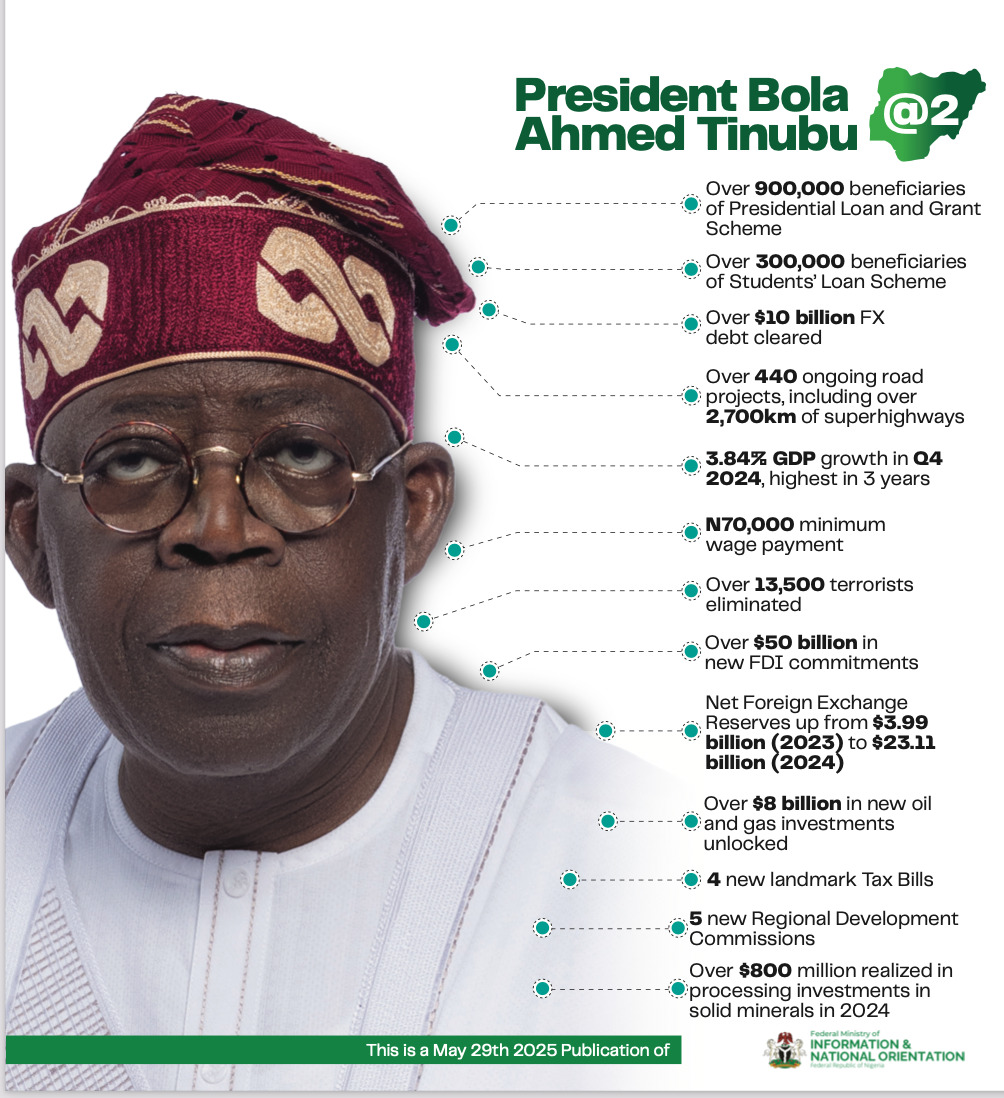
NHIA Director General, Dr Kelechi Ohiri, explained that the move reinforces the Authority’s zero tolerance for poor service delivery under President Bola Tinubu’s vision of Universal Health Coverage for all Nigerians.
“Enrollees deserve the best care and we will continue to do our best to ensure they get it. The sanctions are meant to send a clear message that the NHIA will not tolerate substandard service for enrollees,” Ohiri stated.
He commended diligent healthcare providers who have remained committed to high-quality service, describing them as “worthy partners in our collective journey towards UHC.”
“With the recent actuarial adjustment of capitation and fee-for-service payments to providers the first in 12 years we expect more for patients, not less. We must work together to reduce delays in receiving care,” he added.
To address referral bottlenecks,
The NHIA has now mandated HMOs to issue referral codes within one hour in order to address referral bottlenecks,
The Authority said complaints were received through multiple channels, including in-person visits, emails, phone calls, and the NHIA Call Centre. Complex or unresolved cases were escalated according to its Grievance Management Protocol.
The NHIA emphasized that this accountability drive is part of its broader effort to build trust in the national health insurance scheme, encourage enrolment, and guarantee that every Nigerian receives quality care without fear of denial or exploitation.